Bipolar Disorder
August 16, 2024
Dual Diagnosis
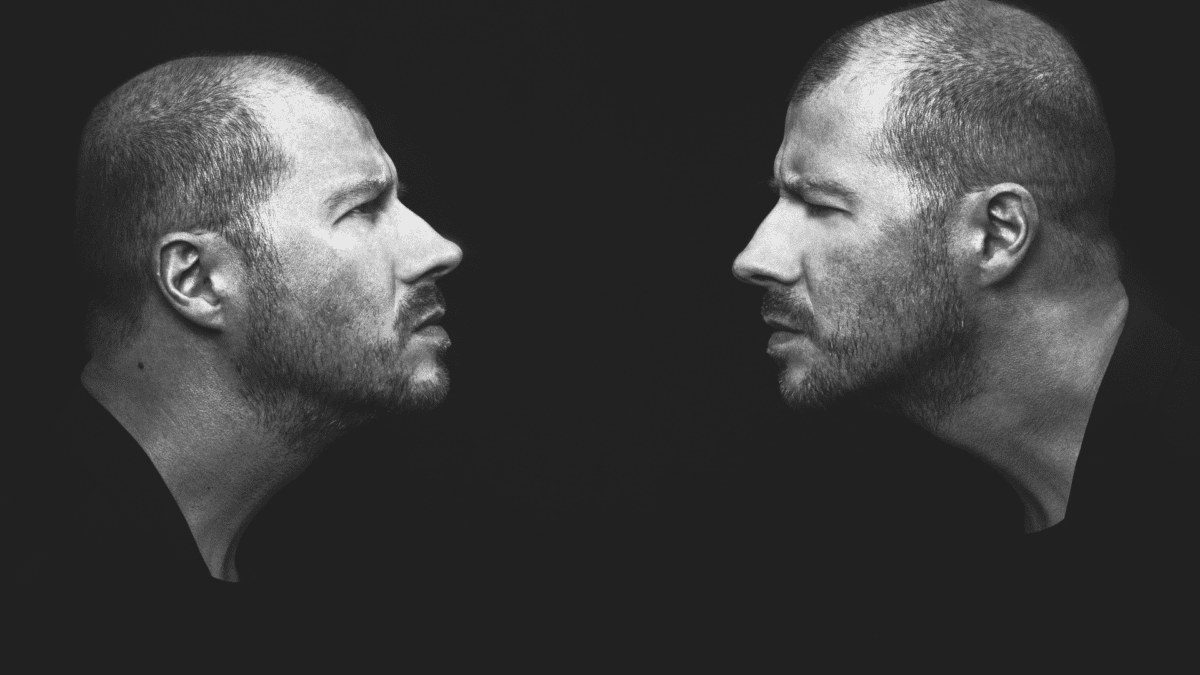
August 16, 2024Living with Borderline Personality Disorder (BPD) can present a range of challenging symptoms that affect an individual’s thoughts, emotions, and behaviors. People with BPD may experience intense mood swings and feel empty or bored easily. They might have difficulty forming stable relationships due to fear of abandonment or rejection.
This intense fear of abandonment triggers anxiety and anger, complicating their interpersonal relationships and leading to erratic behaviors aimed at managing perceptions of closeness and distance in relationships. Impulsivity is another common symptom, leading to risky behaviors like substance abuse or reckless driving.
Individuals with BPD often struggle with a distorted self-image, fluctuating between idealizing and devaluing themselves or others. They might engage in self-harming behaviors as a way to cope with overwhelming emotions. Additionally, chronic feelings of emptiness and anger outbursts can further complicate daily life for those affected by this disorder.
It’s essential to recognize these symptoms early on to seek appropriate treatment and support systems that can help individuals manage their condition effectively.
Causes and Risk Factors of BPD
Many factors can contribute to the development of Borderline Personality Disorder (BPD). It’s believed that a combination of genetic, environmental, and neurological influences play a role in its onset. BPD is a mental illness influenced by these factors.
Genetics may predispose some individuals to BPD, as it is seen to run in families. Traumatic life events such as abuse or neglect during childhood can also increase the risk of developing BPD later in life.
Furthermore, an imbalance in brain chemicals like serotonin, which regulates mood, may be linked to the disorder. Additionally, certain personality traits such as impulsivity and emotional sensitivity are considered risk factors for BPD.
It’s crucial to understand that while these factors may contribute to the development of BPD, each individual’s experience with the disorder is unique and multifaceted.
Diagnosis and Misconceptions about BPD
Diagnosing Borderline Personality Disorder (BPD) can be challenging, as it often involves a comprehensive evaluation by mental health professionals. A borderline personality disorder is diagnosed by reviewing the patient’s health history, family history of mental health issues, and potentially a physical examination to rule out other conditions.
Symptoms such as unstable relationships, intense mood swings, and impulsive behaviors are key indicators of BPD. However, these symptoms can sometimes be misinterpreted or overlooked.
Misconceptions about BPD are common and can lead to stigma and misunderstanding. The stigma associated with personality disorders can significantly affect individuals with BPD, impacting their relationships and self-perception. One prevalent misconception is that individuals with BPD are untreatable or manipulative. In reality, with the right support and treatment, people with BPD can manage their symptoms effectively.
It’s important to address misconceptions surrounding BPD to promote empathy and awareness. By educating ourselves about the disorder and understanding its complexities, we can help create a more supportive environment for those living with BPD.
Treatment Options for BPD
When it comes to treating Borderline Personality Disorder (BPD), there are several options available that can help individuals manage their symptoms and improve their quality of life. It is crucial to emphasize the importance of specialized approaches to treat borderline personality disorder.
Therapy is often a key component in treating BPD, with Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT) being the most commonly used approaches. These therapies focus on helping individuals learn coping skills, regulate emotions, and improve interpersonal relationships.
In addition to therapy, medications may also be prescribed to address specific symptoms associated with BPD, such as mood swings or impulsivity. A borderline personality disorder is treated with various therapeutic approaches such as cognitive behavioral therapy, dialectical behavior therapy, and schema-focused therapy, as well as the potential role of medications to manage specific symptoms like depression and anxiety. It’s essential for individuals with BPD to work closely with a mental health professional to find the right medication regimen that works for them.
Lifestyle changes can also play a significant role in managing BPD symptoms. Engaging in regular exercise, maintaining a healthy diet, getting enough sleep, and avoiding substances like alcohol or drugs can all contribute to the overall well-being of those living with BPD.
Therapy: Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT)
When it comes to treating Borderline Personality Disorder (BPD), therapy plays a crucial role in helping individuals manage their symptoms and improve their quality of life. Two widely used therapies for BPD are Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT).
DBT focuses on teaching individuals skills to regulate emotions, tolerate distress, improve interpersonal relationships, and increase mindfulness. It helps those with BPD develop healthier coping mechanisms and reduce impulsive behaviors.
On the other hand, CBT aims to identify and challenge negative thought patterns and beliefs that contribute to emotional dysregulation. By working with a therapist, individuals can learn how to reframe their thinking and change maladaptive behaviors.
Both DBT and CBT have been shown to be effective in reducing BPD symptoms and enhancing overall well-being. It’s essential for those with BPD to work closely with a mental health professional to determine which therapy approach is best suited for them.
Medications for Borderline Personality Disorder
When it comes to treating Borderline Personality Disorder (BPD), medications can be a helpful component in managing symptoms. While they are not a cure, certain medications may be prescribed by healthcare professionals to address specific aspects of BPD, such as mood swings, impulsivity, and anxiety. In contrast, the treatment of bipolar disorder often involves different medication approaches, focusing on mood stabilizers and antipsychotics to manage the distinct mood fluctuations and overall functioning.
Antidepressants are commonly used to help stabilize moods and reduce feelings of sadness or hopelessness. Mood stabilizers can also be prescribed to manage intense emotional states and impulsive behaviors often associated with BPD. Additionally, antipsychotic medications may be recommended for individuals who experience distorted thinking patterns or paranoia.
It’s important for those considering medication as part of their treatment plan to consult with a psychiatrist or mental health provider. Medication management should always be closely monitored to ensure effectiveness and minimize potential side effects.
Remember that medication is just one piece of the puzzle when it comes to managing BPD. Combined with therapy and lifestyle changes, medications can play a valuable role in promoting overall well-being for individuals living with this condition.
Lifestyle Changes
Making lifestyle changes can significantly impact the management of Borderline Personality Disorder (BPD). Engaging in regular exercise, such as yoga or walking, can help reduce stress and improve overall well-being.
Maintaining a healthy diet rich in fruits, vegetables, and whole grains can also play a crucial role in managing symptoms. Avoiding alcohol and drugs is essential as they can worsen BPD symptoms.
Establishing a consistent sleep schedule is vital for mood regulation and emotional stability. Prioritizing self-care activities like meditation, journaling, or hobbies can provide comfort during challenging times.
Creating boundaries with others to prevent feelings of overwhelm or abandonment is important for individuals with BPD. Building a strong support system of understanding friends and loved ones can offer invaluable emotional support on difficult days.
Incorporating these lifestyle changes alongside therapy and medication options may contribute to better symptom management for those living with BPD.
Coping Strategies for Individuals with BPD
Living with Borderline Personality Disorder (BPD) can be challenging, but there are coping strategies that individuals can implement to help manage their symptoms. It is also important to address co-occurring mental health conditions, such as depression and substance misuse, as part of these coping strategies. One effective strategy is practicing mindfulness and grounding techniques to stay present in the moment and regulate emotions. This can include deep breathing exercises or focusing on sensory experiences like touch or smell.
Another helpful coping strategy is creating a structured routine to provide stability and predictability in daily life. Setting goals, making to-do lists, and establishing a consistent sleep schedule can all contribute to a sense of control and balance. Additionally, engaging in activities that bring joy and relaxation, such as hobbies or creative outlets, can serve as healthy distractions from distressing thoughts or feelings.
Developing strong communication skills is essential for navigating relationships effectively while managing BPD symptoms. Learning how to express needs assertively and set boundaries can improve interactions with others and reduce conflict. Seeking support from trusted friends, family members, or mental health professionals is also vital for building a reliable network of understanding individuals who can offer encouragement during difficult times.
Support Systems for Those with BPD
Navigating Borderline Personality Disorder (BPD) can be challenging, but having a strong support system is crucial for those dealing with this condition. Addressing other mental health conditions that frequently co-occur with BPD, such as depression and substance misuse, is also important in the support process. Family members play a significant role in providing emotional support and understanding to their loved ones with BPD.
It’s essential for family members to educate themselves about BPD to better understand the struggles their loved one may face. By learning more about the disorder, they can offer empathy and compassion, creating a supportive environment.
In addition to family support, therapy can also be beneficial for individuals with BPD. Group therapy or support groups specifically tailored for those with BPD can provide a sense of community and understanding that is invaluable in managing symptoms.
Remember, supporting someone with BPD requires patience and empathy. It’s essential to listen without judgment and validate their feelings even when they may seem irrational. Being there consistently through both good days and bad is key to building trust and stability within the relationship.
Family: Support Systems for Those with BPD
Family plays a crucial role in the support system of individuals with Borderline Personality Disorder. By understanding the challenges and needs of their loved ones, family members can provide invaluable emotional support and encouragement. Communication, empathy, and patience are key when supporting someone with BPD. It is essential to educate oneself about the disorder to offer effective assistance without judgment.
Remember, recovery from Borderline Personality Disorder is possible with the right treatment, dedication, and a strong support system in place. If you or a loved one are struggling with BPD symptoms, seek professional help and lean on your support network for guidance and understanding. Together, we can break the stigma surrounding mental disorders like BPD and foster an environment of compassion and healing.